HEALTH
Improving RAF Scores with Real-Time Documentation Insights from Risk Adjustment Vendors

A Healthcare Provider’s Challenge with Low RAF Scores
Dr. Patel, a primary care physician, had a growing concern—her practice’s Risk Adjustment Factor (RAF) scores were consistently lower than expected. Despite providing comprehensive care, many chronic conditions were being undocumented or misclassified, leading to reduced reimbursements from CMS. With compliance concerns mounting and financial penalties looming, she knew her team needed a better solution.
The issue wasn’t a lack of expertise—it was a documentation gap. By the time coders reviewed patient charts retrospectively, crucial diagnoses had been missed or lacked proper evidence. This not only affected reimbursements but also hindered patient care coordination in value-based care models.
That’s when Dr. Patel’s health network partnered with a Risk Adjustment Vendor offering real-time documentation insights. The impact? Immediate improvements in coding accuracy, risk capture, and compliance—all translating to higher, more accurate RAF scores.
The Shift from Retrospective to Real-Time Risk Adjustment Coding
Traditionally, risk adjustment coding has been a retrospective process, relying on post-visit chart reviews. However, this approach is reactive—by the time missing diagnoses are found, CMS submission deadlines may have passed, or audits may reveal compliance gaps.
Real-time documentation insights powered by AI-driven risk adjustment vendors are changing the landscape. By embedding AI and NLP (Natural Language Processing) tools directly into EHRs, healthcare providers can capture diagnoses accurately at the point of care rather than relying on manual retrospective reviews.
Why does this matter?
- Undocumented or Misclassified Diagnoses Lower RAF Scores: Missing chronic conditions underestimates patient risk, reducing payments.
- CMS Scrutiny on Coding Accuracy: Without real-time validation, providers face increased audit exposure and financial penalties.
- Inconsistent Risk Adjustment Coding Hurts Value-Based Care: Inaccurate RAF scores distort patient stratification, care coordination, and quality incentives.
How Risk Adjustment Vendors Improve RAF Scores with Real-Time Documentation Insights
- AI-Powered Coding Suggestions at the Point of Care
Imagine a physician diagnosing a patient with diabetes during a routine visit. Real-time AI tools scan the EHR and suggest additional HCC codes based on the patient’s history—such as diabetic neuropathy or chronic kidney disease—ensuring complete documentation.
- AI scans clinical notes and suggests risk-adjusted diagnoses in real time.
- Helps providers capture chronic conditions accuratelyduring the patient visit.
- Reduces reliance on manual coding interventions post-visit.
- Pre-Visit Risk Assessments for Proactive Risk Capture
Risk adjustment isn’t just about real-time coding—it’s about anticipating missing diagnoses before the patient even arrives.
- AI-powered pre-visit reviews scan historical EHR data.
- Identifies undocumented conditions and coding gaps before the encounter.
- Providers receive a real-time summary of potential risk factors to ensure complete documentation.
- Automated NLP for Complete Risk Capture
Manual chart reviews are tedious and prone to human error. AI-driven Natural Language Processing (NLP) extracts clinically relevant diagnoses from physician notes, ensuring that nothing is overlooked.
- Scans physician notes for hidden risk factors.
- Reduces manual effort in retrospective reviews.
- Ensures completeness and compliance in HCC coding.
- Compliance-Driven Risk Adjustment Audits
CMS and OIG audits have become more stringent. Without real-time documentation validation, providers face audit risks and reimbursement clawbacks.
- AI audits RAF-related documentation to ensure CMS compliance.
- Flags missing, incomplete, or inconsistent risk-adjusted diagnoses.
- Prevents over- or under-documentation issues before claim submission.
- Seamless Integration with Risk Adjustment Coding Systems
The best solutions are those that integrate seamlessly into provider workflows. Risk adjustment vendors offer EHR-embedded coding prompts, allowing providers to document risk scores effortlessly.
- Aligns clinical documentation, coding teams, and CDI specialists.
- Embeds real-time HCC code suggestions directly into EHRs.
- Reduces the burden of retrospective queries and manual audits.
The Financial and Compliance Benefits of Real-Time Documentation Insights
- Higher RAF Scores for Accurate Reimbursement
- Capturing all chronic conditions ensures providers receive appropriate payments.
- Avoids revenue loss from under-coded diagnoses.
- Reduced Audit Risk and Coding Compliance Errors
- Real-time validation ensures that documentation meets CMS standards.
- Prevents compliance violations and financial clawbacks.
- Enhanced Provider Efficiency and Satisfaction
- Eliminates the need for excessive post-visit queries and retrospective chart reviews.
- Reduces physician burnout by streamlining documentation.
Best Practices for Implementing Real-Time Documentation Solutions
- Train Providers on AI-Driven Documentation Workflows
- Educate clinicians on how real-time coding insights improve risk score accuracy.
- Ensure seamless adoption of AI-powered documentation tools.
- Utilize Pre-Encounter Risk Analysis for Proactive Coding
- Use predictive analytics to identify high-risk patients before each visit.
- Encourage proactive coding adjustments to prevent missed diagnoses.
- Monitor and Validate RAF Score Trends
- Regularly track risk score changes and adjust documentation workflows accordingly.
- Implement audit-proof coding methods to ensure RAF accuracy.
- Ensure Risk Adjustment Vendors Provide AI-Powered Chart Reviews
- Automate detection of uncaptured conditions and documentation inconsistencies.
- Improve HCC coding accuracy with AI-driven NLP audits.
- Align Risk Adjustment Coding with Value-Based Care Strategies
- Ensure risk capture supports population health management and patient stratification goals.
- Use AI-driven risk models to prioritize preventive care initiatives.
The Future of Risk Adjustment Coding with AI-Driven Real-Time Documentation
- Greater Automation for Risk Score Validation: AI will continue to enhance real-time documentation accuracy.
- Deeper Integration of Predictive Analytics: Expect more precise RAF score forecasting to optimize reimbursements.
- Stronger Alignment with Value-Based Payment Models: Risk capture will directly impact care quality and financial incentives.
Final Thoughts: Actionable Steps for Healthcare Organizations
- Evaluate Current RAF Optimization Strategies – Identify documentation inefficiencies and coding gaps.
- Adopt AI-Powered Risk Adjustment Vendor Solutions – Ensure seamless integration of real-time documentation insights.
- Develop a Proactive Risk Score Management Plan – Implement pre-visit coding assessments and AI-driven NLP audits.
- Monitor Reimbursement Performance and Compliance Trends – Track RAF score improvements, financial gains, and audit risk reduction.
Closing Thoughts
Risk Adjustment Vendors play a critical role in ensuring real-time documentation accuracy, improving RAF scores, reducing audit risks, and securing accurate reimbursements. By integrating AI-powered risk adjustment solutions, providers can confidently navigate the evolving healthcare reimbursement landscape while focusing on what matters most—delivering quality patient care.
HEALTH
What Is a SLAP Tear? Understanding This Common Shoulder Injury
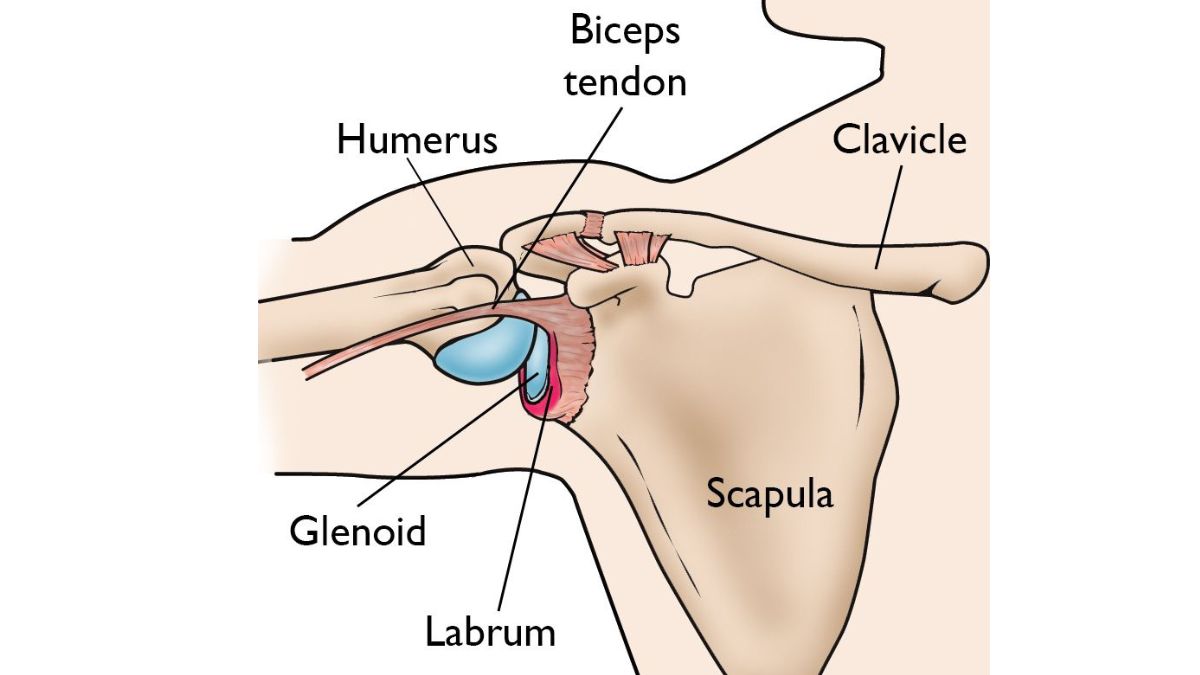
If you’ve been experiencing shoulder pain, clicking, or a loss of strength—especially during overhead movements—you may be dealing with more than just a strain. One possible culprit is a SLAP tear, a specific type of injury to the shoulder joint that can affect everyone from athletes to weekend warriors.
What Does “SLAP Tear” Mean?
SLAP stands for Superior Labrum Anterior and Posterior. In simpler terms, it’s a tear in the top part of the labrum—the ring of cartilage that surrounds the socket of your shoulder joint. This cartilage helps stabilize your shoulder and keep the ball of your upper arm bone in place. When torn, the result can be instability, discomfort, and reduced mobility.
How Does a SLAP Tear Happen?
SLAP tears can result from either acute trauma or repetitive motion. Some of the most common causes include:
- Falling on an outstretched arm
- Lifting heavy objects or weights with poor form
- Repetitive overhead movements (common in baseball, swimming, tennis, etc.)
- Sudden pulling motions (like grabbing something while falling)
In some cases, SLAP tears can also be part of the natural wear-and-tear process, especially in people over 40.
Common Symptoms of a SLAP Tear
Not all SLAP tears feel the same, but here are some symptoms to watch for:
- Deep shoulder pain, especially during overhead activity
- A clicking or popping sensation
- Weakness or fatigue in the shoulder
- Limited range of motion
- A feeling that your shoulder is going to “slip out”
These symptoms often mimic other shoulder conditions, which is why getting an accurate diagnosis is so important.
Diagnosing a SLAP Tear
A shoulder specialist will typically begin with a physical exam and a review of your activity history. Imaging tests like an MRI can help confirm the diagnosis, though in some cases, an arthroscopic procedure may be necessary to fully visualize the tear.
For a deeper dive into how SLAP tears are diagnosed and treated, visit: https://levelupshoulder.com/slap-tears/
Treatment Options
Treatment depends on the severity of the tear and your activity level. In mild cases, rest, anti-inflammatory medications, and physical therapy may be enough to restore function. For more serious tears—especially in younger or highly active individuals—arthroscopic surgery may be recommended to repair the torn labrum.
Post-surgery, a rehabilitation program will help restore range of motion, rebuild strength, and reduce the risk of reinjury.
Don’t Ignore Shoulder Pain
A SLAP tear can seriously impact your ability to perform daily tasks and enjoy physical activity. If you’re experiencing persistent shoulder pain, especially with overhead movements, it’s worth getting it checked out. Early treatment leads to better outcomes and a quicker return to the things you love.
HEALTH
What Is Orthopedic Medicine? An Intro to Bone and Joint Health

From sore knees after a weekend hike to a torn rotator cuff that just won’t heal, many of us deal with bone, joint, or muscle pain at some point in our lives. That’s where orthopedic medicine comes in. But what exactly does it cover—and when should you see an orthopedic specialist?
Whether you’re an athlete, a weekend warrior, or simply want to stay mobile and pain-free as you age, understanding the basics of orthopedic care can help you make better decisions about your health.
What Is Orthopedic Medicine?
Orthopedic medicine is a branch of medicine focused on the musculoskeletal system, which includes your bones, joints, ligaments, tendons, muscles, and nerves. The goal is to diagnose, treat, and prevent injuries and disorders that affect movement, stability, and function.
Orthopedic specialists, also known as orthopedists or orthopedic surgeons, are trained to handle everything from acute injuries (like fractures and dislocations) to chronic conditions such as arthritis, tendonitis, and degenerative joint disease.
What Conditions Do Orthopedic Doctors Treat?
Orthopedic medicine covers a wide range of conditions affecting different areas of the body, including:
- Shoulder injuries: rotator cuff tears, labral tears, impingement
- Knee issues: ACL tears, meniscus injuries, runner’s knee, arthritis
- Spine problems: herniated discs, sciatica, scoliosis
- Hip pain: bursitis, labral tears, osteoarthritis
- Hand and wrist: carpal tunnel syndrome, fractures, tendonitis
- Foot and ankle: plantar fasciitis, sprains, Achilles tendon injuries
Many of these conditions can be treated with non-surgical methods, though surgery may be necessary in more severe cases.
Types of Orthopedic Care
Orthopedic care includes both surgical and non-surgical options, depending on the injury or condition. Treatment approaches may involve:
- Physical therapy and rehabilitation
- Injections (such as cortisone or PRP) to reduce inflammation and pain
- Bracing or casting for stability and healing
- Minimally invasive surgery, like arthroscopy
- Joint replacement surgery, typically for hips, knees, or shoulders
For example, orthopedic treatments by Level Up Shoulder, Dr. Drake focus not only on surgical repair of shoulder injuries, but also on functional rehab, strength restoration, and getting patients back to the activities they love—faster and stronger.
When Should You See an Orthopedic Doctor?
If you’re experiencing any of the following, it may be time to schedule a consultation:
- Persistent joint or muscle pain
- Swelling or stiffness that doesn’t improve with rest
- Limited range of motion in a joint
- Weakness or instability
- An injury that isn’t healing properly
- Pain that interferes with your daily life or sleep
Early intervention can prevent long-term damage and get you back to full strength sooner.
Conclusion
Orthopedic medicine plays a vital role in keeping your body moving the way it should. Whether you’ve suffered a sports injury or are dealing with years of wear and tear, orthopedic specialists are trained to help you regain mobility, reduce pain, and improve your quality of life.
From preventive care to advanced surgical procedures, orthopedic treatments are designed to keep your bones and joints working better, for longer.
HEALTH
Raising Healthy Smiles: The Essentials of Pediatric Dental Care

What Is Pediatric Dentistry?
In addition to providing dental care, pediatric dentistry promotes good oral hygiene from an early age. Unlike general dentistry, pediatric dentists focus on young patients’ unique challenges and considerations. Their specific training prepares them to prevent and treat oral health problems in newborns, kids, and teenagers. Facilities like a Pediatric Dentist in Thornton provide environments specifically designed for children, helping ease anxiety and making dental visits enjoyable experiences. A pediatric facility’s vibrant and entertaining surroundings can significantly influence a child’s desire to get dental care.
The Importance of Early Dental Visits
Starting dental visits early is an investment in lifelong oral health. These initial visits, as recommended by the American Academy of Pediatric Dentistry, set the stage for understanding the importance of dental care. These are crucial periods when dentists can introduce children to oral hygiene and the significance of caring for their teeth. By capturing a child’s interest and removing any fear associated with dental visits, these experiences contribute to effectively monitoring and guiding the development of both baby and permanent teeth.
Understanding Common Pediatric Dental Issues
Children’s dental problems, including cavities and gum disease, are sometimes written off as trivial, but if ignored, they can cause serious health problems. Children are prone to cavities due to the sugary foods they consume and their sometimes irregular brushing habits. In addition, behaviors like thumb-sucking and extended use of pacifiers can affect tooth alignment and jaw development. By attending regular dental visits, parents can gain insights from dental professionals on mitigating these risks and ensuring early intervention. A more secure oral future can result from early detection of these disorders, which can stop them from developing into more serious tooth health difficulties.
Tips for Promoting Healthy Dental Habits
Creating a routine around dental care can help instill lifelong habits in children. They must be taught to use fluoride toothpaste and clean their teeth twice daily. Flossing should also be incorporated once teeth begin to touch. These habits need reinforcement at home to foster a sense of accountability in children. Parents can use visual aids or reward systems as positive reinforcements. Demonstrating proper techniques adds value, as children are likely to imitate the actions they observe. Good oral hygiene should be framed positively as an empowering practice rather than a chore.
Nutrition’s Role in Oral Health
A balanced diet is a pillar of strong oral health. Foods containing essential minerals, particularly calcium and phosphorus, are crucial in maintaining healthy enamel and oral well-being. Nuts, leafy greens, and dairy products can all significantly improve tooth health when consumed regularly. It’s also critical to restrict the consumption of acidic drinks and sugary foods that cause cavities. The resource on WebMD highlights the importance of a balanced diet in protecting your child’s teeth. Making informed choices about diet is an impactful way for parents to exercise control over their child’s oral health outside of the dental office.
How to Choose the Right Pediatric Dentist
Choosing a pediatric dentist shouldn’t be rushed. It’s a decision that can influence a child’s view of dental care. A pediatric dentist’s ability to communicate effectively with children and a friendly, inviting office atmosphere can make visits less intimidating. You could feel more at ease reading online reviews or asking friends for recommendations. The right dentist will engage with children in a way that builds trust and encourages enthusiasm for dental care. Parents are encouraged to visit potential dental practices to assess the environment and ensure it aligns with their child’s comfort levels and needs.
Setting Up a Child-Friendly Dental Routine
Making dental hygiene a habitual, positive practice begins with creativity. Utilizing tools such as songs, colorful toothbrushes, or even digital apps tracking brushing time can turn routine into fun. Allowing your child to pick out their dental supplies can also foster a sense of ownership over their oral hygiene. Establishing a routine, like brushing after breakfast and before bed, helps to weave dental care seamlessly into daily life. Consistency is key, and positive reinforcement can encourage a child to see these activities as enjoyable and rewarding.
Navigating Dental Anxiety in Children
Dental anxiety can significantly impact a child’s willingness to receive care, but it can be managed successfully. Introducing your child to the dental office gradually and supportively can alleviate fear. Explaining dental procedures using child-friendly language and offering reassurance can demystify the experience. Techniques such as deep breathing exercises or storytelling can divert attention, making visiting less daunting. Creating a supportive environment at home and during dental visits cultivates a positive attitude toward long-term dental wellness.
-

 BLOG1 year ago
BLOG1 year agoATFBooru: A Hub for Animated Art and Community
-

 CONSTRUCTION1 year ago
CONSTRUCTION1 year agoBuilding a Home Gym in Your Basement (7 Key Renovation Tips)
-

 BLOG1 year ago
BLOG1 year agoFictionmania: A Deep Dive into the World of Transformative Stories
-

 GAMES1 year ago
GAMES1 year agoSnow Rider 3D: Unblocked Tips and Tricks for Gamers
-

 LIFESTYLE1 year ago
LIFESTYLE1 year agoVersatile Living: Stylish Indoor Outdoor Rugs with Eco-Friendly Appeal
-

 BLOG1 year ago
BLOG1 year agoGIFHQ: A Comprehensive Guide
-

 LIFESTYLE1 year ago
LIFESTYLE1 year agoAchieve Elegance with Chic Blue Formal Dresses and Redken Professional Hair Care for All Hair Types
-
 BLOG1 year ago
BLOG1 year agoVincent herbert new wife: A Detailed Overview
